https://philaholisticclinic.com/narcolepsy-treatment/
Holistic Treatment for Narcolepsy
Narcolepsy treatment
Narcolepsy treatment is complex and not always successful. There is no cure for narcolepsy in traditional medicine, but medications and lifestyle modifications can help you manage your symptoms.
The particular treatment approach will be decided by your medical practitioner based on:
- age,
- physical condition,
- medical history
- the severity of the symptoms
- your tolerance to certain drugs, procedures, or therapies
- your expectations from the course of treatment
- your belief, attitude, and preference
The goal of narcolepsy treatment is to help you stay as alert as possible throughout the day. It is also important to reduce the time you lose muscle control. In an ideal world, this can be accomplished using a minimal quantity of medicines.
- medications.
For excessive sleepiness, central nervous system stimulants are usually prescribed. Antidepressants can help with muscle control.
- nap therapy.
Two or three short naps during the day can help control sleepiness and maintain alertness.
- right nutrition
- regular training
- behavior therapy
Narcolepsy is not curable in western medicine. The Food and Drug Administration has approved a drug called modafinil to treat excessive daytime sleepiness. Two classes of antidepressants – tricyclic antidepressants and selective serotonin reuptake inhibitors – have been shown to be effective in controlling cataplexy in many patients. Pharmaceutical treatment should be accompanied by behavioral therapies. Many people with narcolepsy regularly take short naps at times when they feel most sleepy. Improving the quality of sleep at night can counteract excessive daytime sleepiness and alleviate persistent feelings of tiredness.
None of the medications currently available allow people with narcolepsy to maintain their full normal level of alertness over the long term. But excessive daytime sleepiness and cataplexy, the most disabling symptoms of the condition, can be controlled with drug narcolepsy treatment in most patients. It is important to modify the narcolepsy treatment regimen as symptoms change.
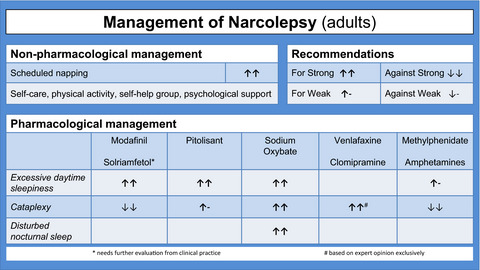
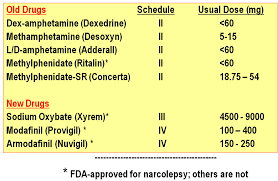
Medications for narcolepsy treatment
Stimulants.
Central nervous system stimulants are the primary medications for narcolepsy that help people stay awake during the day. Doctors often try modafinil (Provigil) or armodafinil (Nuvigil) first to treat narcolepsy. Modafinil and armodafinil are not as addictive as older stimulants and do not cause the ups and downs that are often associated with older stimulants. Side effects are rare but can include headache, nausea, or anxiety.
Sunosi (solriamphetol) and pitolisant (Wakix) are newer stimulants used in narcolepsy, headache, and anxiety. Pitolisant can also be helpful with cataplexy.
Some people need treatment with methylphenidate (Aptensio XR, Concerta, Ritalin, others) or with various amphetamines. These medications for narcolepsy are very effective but can be addictive. They can cause side effects such as nervousness and palpitations.
(SSRIs) – Selective serotonin reuptake inhibitors and (SNRIs) – serotonin and norepinephrine reuptake inhibitors.
Doctors often prescribe these medications for narcolepsy, which suppresses REM sleep, to relieve symptoms of cataplexy, hypnagogic hallucinations, and sleep paralysis. These include fluoxetine (Prozac, Sarafem) and venlafaxine (Effexor XR). Side effects from the use of this group of medications may include weight gain, restlessness, and gastrointestinal problems.
Tricyclic antidepressants.
These older antidepressants, such as protriptyline (Vivactil), imipramine (Tofranil), and clomipramine (Anafranil), are effective for cataplexy, but many people complain of side effects such as dry mouth and dizziness.
Sodium oxidate (Xirem).
This remedy is very effective in catalepsy. Sodium oxidate helps improve nighttime sleep, which is often poor in narcolepsy. In high doses, it can also help control daytime sleepiness. It should be taken in two doses: one at bedtime and one four hours later.
If you are suffering from any other health problems, such as high blood pressure or diabetes, ask your doctor how the medications you take for your other conditions may interact with those taken for narcolepsy.
Some over-the-counter medications, such as allergy and cold medications, can cause drowsiness. If you are suffering from narcolepsy, your doctor will likely advise you to avoid taking these medications.
Emerging treatments being studied for narcolepsy include medications for narcolepsy that affect the chemical histamine system, hypocretin replacement, hypocretin gene therapy, and immunotherapy, but more research is needed before they can be available in the doctor’s office.
What is narcolepsy?
Narcolepsy is a neurological medical condition that impacts the brain’s ability to control sleep and alertness. If you are suffering from narcolepsy, you experiencing excessive daytime drowsiness or even somnolence as well as uncontrollable episodes of daytime lethargy. These sudden sleep attacks can occur with any activity and at any time of the day.
Approximately one in 2,000 Americans are suffering from narcolepsy. The disorder affects men and women equally. Up to 10% of people who have narcolepsy have a relative who also has the disorder. Narcolepsy occurs in people of all ages, but the first sign of daytime sleepiness usually appears in the teens or twenties. For the reason that the symptoms of narcolepsy may simulate depression, chronic fatigue syndrome, or other medical conditions, it can go undiagnosed and untreated for years.
In this article Dr. Tsan will share his academic and clinical experience and convey his knowledge on:
- What is narcolepsy?
- What are the causes of narcolepsy?
- Symptoms of narcolepsy?
- Types of narcolepsy?
- Natural treatment for narcolepsy, and more.
The first signs that may make you consider that you are suffering from narcolepsy are shown in the table below.
| People with narcolepsy | People without narcolepsy |
During the day | |
| Feel tired, distracted, and fall asleep effortlessly | Feel alert, conscious, and don’t instantly fall asleep |
| Frequently enter REM nap and dreaming for the duration of periods of sleep | Normally do not enter REM napping and don’t dream throughout sleep |
| Hallucinations on awakening are common | Hallucinations on waking up are unusual |
| Sleep unresponsiveness is common | Sleep palsy is uncommon |
| May go through cataplexy | Never encounter cataplexy |
During the night | |
| Unexpectedly wake from sleep | Mostly sleep well |
| Entering the REM sleep within 15 minutes | Begin in a non-REM nap and then after 1 to 1.5 hours enter REM sleep |
Narcolepsy is a neurological disorder that causes persistent drowsiness and additional symptoms such as brief episodes of muscle weakness known as cataplexy, vivid and dream-like hallucinations, short episodes of paralysis when falling asleep or waking up (sleep paralysis), and fragmented nighttime sleep. Symptoms usually develop over several months and persist throughout life.
The disorder usually begins between the ages of 10 and 20, although it sometimes begins before the age of 40 or 50. Narcolepsy affects women and men equally, affecting about 1 in 2,000 people.
Narcolepsy is a manageable condition, and with the help of a range of therapeutic strategies, people with narcolepsy can lead full and satisfying lives.
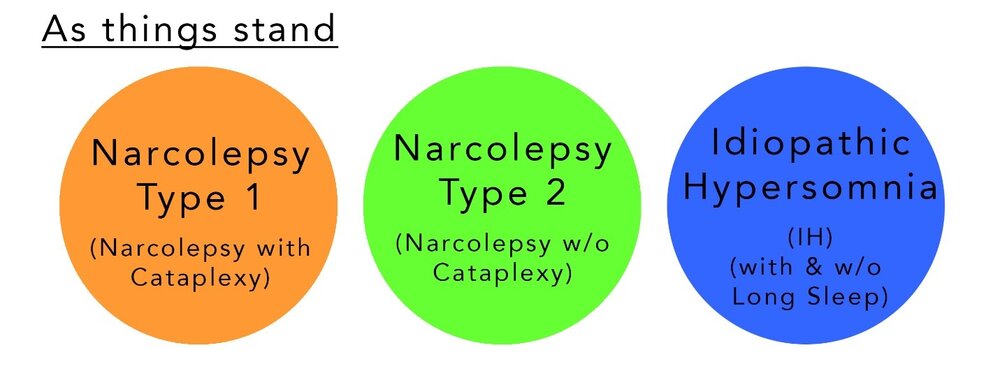
Types of narcolepsy
There are three major types of narcolepsy recognized by clinicians:
Type 1 aka NT1 – formerly called narcolepsy with cataplexy.
Individuals with type 1 narcolepsy have excessive daytime sleepiness plus cataplexy and/or low levels of a chemical called hypocretin in the brain.
The research defines it as a state of marked loss of voluntary movement, in which the limbs remain in whatever position they are in.
Sudden muscle weakness or loss of muscle tone is caused by strong emotions such as laughter, winning a game, or sometimes anger.
- cataplexy attacks
- sleep paralysis
- hallucinations
- disturbed sleep
- Begins in childhood or adolescence, requires lifelong treatment
- Rapid eye movements (rapid eye movement) and parasomnias during non-REM sleep.
- high blood pressure at night
Other related disorders are:
- weight gain,
- diabetes,
- sleep apnea,
- heart problems,
- mood swings,
- nervousness,
- sadness,
- eating disorders,
- HDD,
- restless legs.
Type 2 aka NT2 – formerly known as narcolepsy without cataplexy.
Individuals with type 2 narcolepsy have excessive daytime sleepiness but no cataplexy and normal hypocretin levels.
All of the above symptoms not including catalepsy are classified as type 2 narcolepsy.
In short, the complexity of treatment lies in the fact that the prevalence of type 2 and its effect on bodily functions is still unknown or unclear. In addition, the heterogeneity of the condition leads to type 1 symptoms in some patients even without catalepsy.
Other symptoms of narcolepsy type 2 are:
- sleepiness during the day
- frequent awakenings during the night
- sudden brief bouts of drowsiness or falling asleep suddenly
- brief paralysis on awakening
- automatic behavior – doing something unintentionally or automatically
Secondary narcolepsy
This is another very rare type of narcolepsy, which occurs with a lesion in a deep part of the brain called the hypothalamus. In addition to any of the typical symptoms of narcolepsy, people with secondary narcolepsy also have severe neurological problems and require large amounts (> 10 hours) of sleep.
Cataplexy and Catalepsy
According to the Sleep Foundation, patients diagnosed with NT1 often experience episodes of cataplexy. But not observed in NT2 patients.
Unlike catalepsy, cataplexy is sudden muscle weakness during wakefulness, usually triggered by positive expressions such as laughter, conversation, amazement, etc.
On the other hand, catalepsy causes stiffness, loss of consciousness, or sensation.
The causes of cataplexy are still being researched, loss of orexin (hypocretin) leads to disruption of sleep-wake cycles. Also, the most important feature of cataplexy is that it is not always associated with narcolepsy, but it can cause other genetic disorders such as strokes, brain tumors, Niemann-Pick type C disease (NPC), Prader-Willi syndrome, and Angelman syndrome.
Diagnosis of narcolepsy
Narcolepsy is diagnosed after your health care provider performs a detailed medical and sleep history, physical exam, medication history, and sleep studies (which are done at a sleep disorders center). You may also be asked to wear a wrist motion sensor (called an actigraph) for a few weeks or to keep a sleep diary, which involves recording how easy it is for you to fall and stay asleep, how many hours of sleep you get each night and how awake you feel during the day.
Your doctor may make a provisional diagnosis of narcolepsy based on excessive daytime sleepiness and sudden loss of muscle tone (cataplexy). Following a preliminary diagnosis, your practitioner may refer you to a sleep consultant for additional assessment.
Formal diagnosis requires an overnight stay at a sleep center for in-depth sleep analysis by sleep experts. Methods for diagnosing narcolepsy and determining its severity include:
Sleep history.
Your doctor will ask you to provide a detailed sleep history. Part of the story involves completing the Epworth Sleepiness Scale, which uses a series of short questions to rate how sleepy you are. For example, you indicate on a numerical scale how likely you are to doze off in certain situations, such as sitting down after dinner.
Sleep logs.
You may be requested to carry out a complete diary of your sleep pattern for a week or two so your physician can evaluate how your sleep pattern and alertness are linked.
Often, in addition to this sleep record, the doctor will ask you to use an actigraph. This device has the appearance of a wristwatch. It determines periods of activity and sleep and discovers a secondary measure of how and when you sleep.
Polysomnography.
This test measures a variety of signals during sleep using electrodes placed on the scalp. For this test, you must spend one night in a medical facility. The test measures the electrical activity of the brain (electroencephalogram) and heart (electrocardiogram) and the movement of muscles (electromyogram) and eyes (electrooculogram). It also monitors your breathing.
Multiple sleep latency test.
Multiple sleep latency tests determine how long it takes for an individual to fall asleep in the course of the day. You will be asked to take four or five naps, each two hours apart. The specialists will observe your sleep patterns. People with narcolepsy fall asleep easily and quickly enter REM sleep.
These tests can also help medical practitioners to rule out other potential sources of a patient’s symptoms. Other sleep disorders, such as chronic sleep deprivation, the use of sedative medications, and sleep apnea, can cause excessive daytime sleepiness.
What are the causes of narcolepsy?
Many cases of narcolepsy are thought to be caused by a deficiency in a brain chemical hypocretin aka orexin, which regulates sleep. Hypocretin is important in regulating the sleep/wake cycle, including the state of rapid eye movement (REM) sleep. A shortage of hypocretin causes excessive sleepiness, and the characteristics of REM sleep (also called “dream sleep”) become present during wakefulness.
The deficiency of orexin is believed to be the outcome of the immune system that erroneously attacks sections of the brain that produce orexin. Scientists call this kind of reaction – autoimmune reaction.
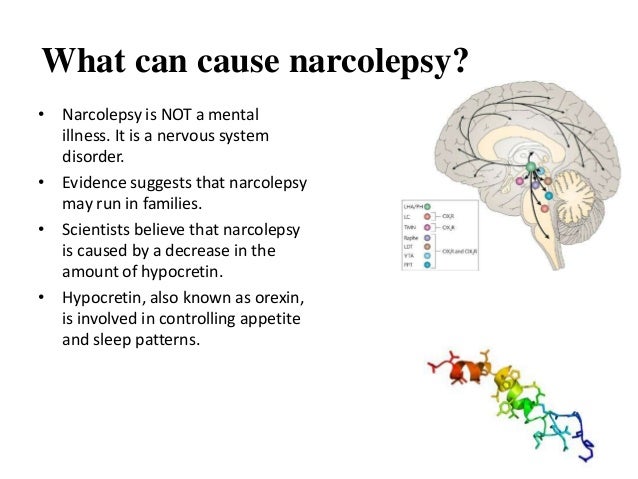
But not in all cases, the causes of narcolepsy are linked to a lack of orexin.
Other possible factors scientists believe play a role in narcolepsy are:
- Family history. Some people with narcolepsy have close relatives with similar symptoms.
- Traumatic brain injury or tumor. In a small number of patients, the area of the brain that controls REM sleep and wakefulness may be damaged by injury, tumor, or disease.
- Environmental toxins such as pesticides, heavy metals, and secondhand smoke.
- Hormonal changes, including those that take place during puberty or menopause
- Chronic mental stress
- Sudden change in sleep pattern
- Infection diseases such as swine flu or a strep throat
- Side effect from the use of flu vaccine Pandemrix
Research conducted in 2013 found an association between the Pandemrix influenza vaccine, which was used during the 2009–2010 swine flu epidemic, and narcolepsy in children.
The risk is very low, with the chance of developing narcolepsy after a dose of the vaccine estimated to be about 1 in 52,000.
But Pandemrix is no longer used in the UK for flu vaccinations.
What are the symptoms of narcolepsy?
Not everyone would experience the same symptoms of narcolepsy. Some people have symptoms regularly, others are affected less frequently.
Symptoms of narcolepsy can develop slowly over several years or suddenly over the course of a few weeks.
Narcolepsy is usually a long-term (chronic) condition, although some of the narcolepsy symptoms may improve with age.
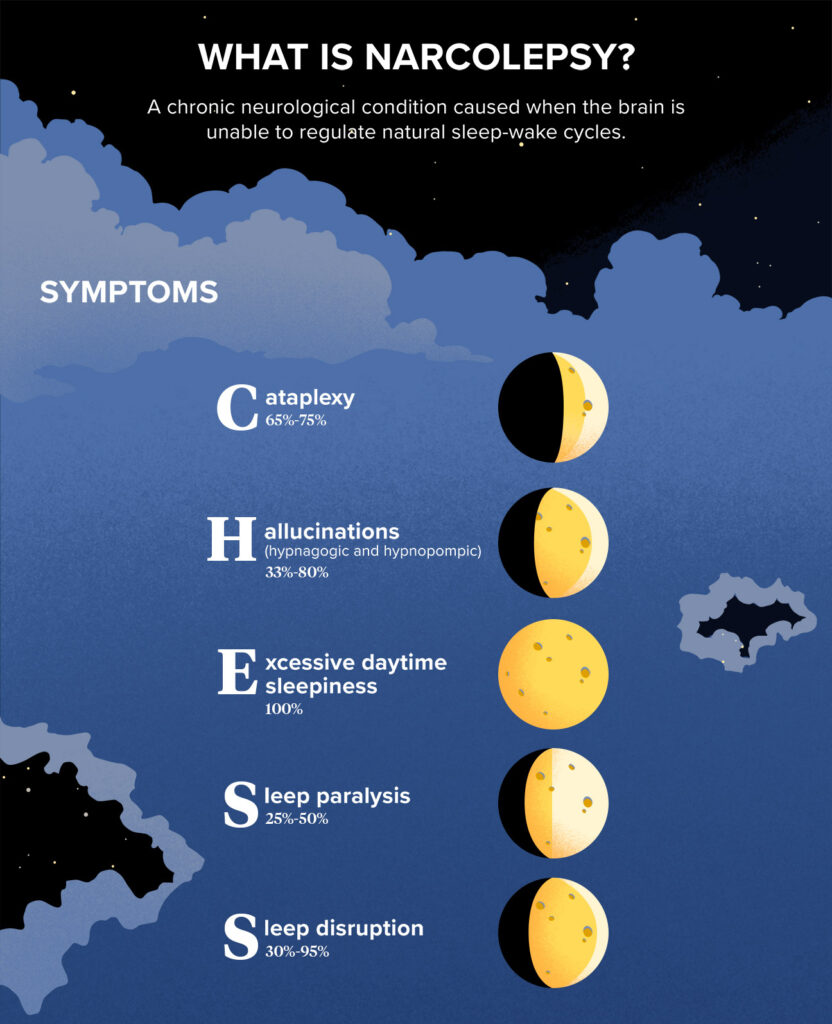
Excessive daytime sleepiness
Excessive daytime sleepiness is usually the number one sign on the list of narcolepsy symptoms. These symptoms of narcolepsy can make a major impact on a person’s daily living routine.
Feeling sleepy during the day and having difficulty falling asleep make it difficult to concentrate at work or school.
People with narcolepsy may be misjudged as lazy or rude.
Sleep attacks
Sleep attacks, during which you fall asleep suddenly and without warning, are also one of the most common narcolepsy symptoms. Those sleep attacks can happen at any time.
The duration of a sleep attack will vary from person to person. Some people have “micro-sleep” lasting only a few seconds, while others may fall asleep for a few minutes.
If narcolepsy is not well controlled, sleep attacks can happen several times a day.
Cataplexy
Most people with symptoms of narcolepsy also experience cataplexy. Cataplexy is a sudden temporary episode of muscle weakness or loss of control over the muscle. These symptoms of narcolepsy are specific for Narcolepsy type 1 – formerly called narcolepsy with cataplexy.
Typical symptoms of narcolepsy with cataplexy are:
- the drooping jaw
- the head that goes down
- legs collapsing uncontrollably
- slurred speech
- double vision or difficulty focusing
Attacks of narcolepsy with cataplexy are typically initiated by vigorous emotional conditions, such as excitement, laughter, anger, or surprise.
Attacks of narcolepsy with cataplexy can last from several seconds to a number of minutes.
Some people with narcolepsy have bouts of cataplexy once or twice a year, while others experience them multiple times a day.
In an effort to avoid attacks, some people can become emotionally withdrawn and socially isolated.
Sleep paralysis
Certain people with narcolepsy encounter incidents of sleep paralysis. This is a temporary inability to move or speak that occurs when you wake up or fall asleep.
Similar to attacks of narcolepsy with cataplexy Outbreaks of sleep paralysis may last from several seconds to several minutes. Although sleep paralysis does no harm, not being able to move can be frightening.
Other common symptoms of narcolepsy are:
- hallucinations – seeing or hearing unreal things, especially when falling asleep or waking up; being in the bedroom is the most common hallucination
- memory problems
- headache
- restless sleep—for example, hot flashes, frequent awakenings, vivid nightmares, or the physical manifestation of dreams
- automatic behavior – continuation of an action without any recollection of it afterward
- depression
Natural treatment for narcolepsy
Lifestyle changes are important in managing the symptoms of narcolepsy. Any approaches to Natural narcolepsy treatment should begin with changes in environment and lifestyle. You can benefit from the following steps:
- Frequent, short sleep – evenly distribute them throughout the day; a general practitioner or sleep specialist can help you plan a schedule that fits with your other activities.
- Stick to a schedule. Set your bed and wake up time and keep them the same every day, including Saturdays and Sundays.
- Take a nap. Schedule short naps at regular intervals. A 20-minute nap at a strategic time during the day can refresh and reduce sleepiness by one to three hours. Some people may need longer sleep.
- Avoid nicotine and alcohol. Using these substances, especially at night, may make your symptoms worse.
- Exercise regularly. Moderate regular exercise at least four to five hours before bed can help you feel more alert during the day and sleep better at night. do not exercise too close to sleep – there should be at least 2 hours between the end of a workout and going to bed
- Relaxation before bed – for example, take a warm bath.
- Providing a comfortable sleeping environment – for example, keeping the bedroom at a comfortable temperature, quiet, and free from distractions
- Avoid caffeine (found in coffee, tea, and some carbonated drinks), alcohol, and smoking before bed
- Don’t eat large, heavy meals before bed
What vitamins can help with narcolepsy treatment?
In a 2011 study, there is an indication that narcolepsy patients have a high vitamin D deficiency.
Therefore, the intake of foods rich in vitamin D may be a suggestion to integrate with other medications.
Likewise, the vitamin B complex is important in regulating sleep-wake cycles.
Plan your diet well with a healthy blend of complex carbohydrates, lean proteins, vitamins, and healthy fats that can significantly improve your health. Keep a journal of your diet that can give you a chance, make you feel good, and support your health.
Acupuncture treatment for narcolepsy
The role of acupuncture for narcolepsy is primarily to control the symptoms of the disorder. The treatment involves the treatment of scalp acupuncture points, meridian points (to improve the condition of the spleen), and also auricular acupuncture which is effective in creating neurotransmitters. The disorder of narcolepsy is thought to be caused by a deficiency of the spleen. Improving the function of the spleen will improve the flow of yang qi to the head and remove accumulated phlegm. The combined treatment of scalp, auricle, and spleen strengthening can effectively treat narcolepsy.
The theory of acupuncture and oriental medicine cites many reasons why sleep-wake cycles can be disturbed. In the case of hypersomnia, the source of the problem may be related to the liver organ and blood flow. This may seem rather strange, but the following explanation will help clarify the situation.
One of the great texts of ancient China, The Great Compendium of Acupuncture and Moxibustion, states that “the liver stores blood and the heart move it. If a person moves in a waking state, then the blood is distributed through all channels; the person is resting, the blood is returning to the liver.” A channel or meridian is an invisible path that carries and distributes energy throughout the body.
Treatment for narcolepsy by acupuncture and oriental medicine practitioner will then focus on relieving excess heat from the liver through acupuncture. When the liver cools, it will once again begin the timely release of blood along the meridians of the body, allowing a person to wake up refreshed. The particular acupuncture points will be defined by the severity of the heat. If extreme heat is present, a point with the ability to “drain the fire” can be used.
If you find that you spend too much time napping in bed or napping on the couch without ever feeling ready for the day, consult with your acupuncture and oriental medicine doctor to discuss your concerns.
Narcolepsy treatment in homeopathy
Homeopathic medicines can offer symptomatic help in the management of cases of narcolepsy. These medications are of natural origin and are very safe and effective in helping to gradually reduce the frequency of the complaint. They can be taken along with conventional treatment to help control symptoms. The use of these drugs is recommended in cases of mild to moderate intensity. You should take any of them under the guidance of a homeopathic doctor after a detailed case study and never self-medicate.
Nux Moschata – #1 homeopathic remedy for narcolepsy treatment
Nux Moschata is prepared from the powdered seeds of a plant called Myristica commonly known as nutmeg. It belongs to the Myristicaceae family. It is a prominent drug for the treatment of these cases. People who need it have irresistible drowsiness and drowsiness. They’re sleepy like they’re drunk. This can be accompanied by vertigo. With drowsiness, excessive laughter may be present. After waking up, a strange sensation is felt. They tend to start off in sleep with a jolting sensation as if electricity is passing through the body.
Gelsemium – one of the best homeopathic remedies for narcolepsy associated with drowsiness and long, sound sleep
It is made from the bark of the root of the Gelsemium Sempervirens plant, commonly known as yellow jasmine. This plant belongs to the Loganiaceae family. This drug is well suited for those who suffer from drowsiness and long, sound sleep. Fear of moving when drowsy. You are usually restless at night towards morning. You feel dull and have trouble directing your attention. It is also used when drowsiness is felt while studying.
Mercurius Solubilis – effective Natural treatment for narcolepsy when excessive sleepiness is not relieved by long sleep
Mercurius Solubilis is useful in cases where a person has great daytime sleepiness that is not relieved even from a long sleep. At night, insomnia or very light sleep with frequent awakenings. There is restless sleep. After waking up, there is a nervous tremor.
Antimonium Tartaricum – one of the best homeopathic remedies for narcolepsy accompanied with unstoppable drowsiness
Antimonium Tartaricum is recommended when a person has insurmountable drowsiness. There is an urgent need for sleep during the day. There is excessive yawning. There are jerks in the body during sleep. Talking or crying while sleeping occurs. There is restlessness and insomnia at night with restless tossing. In the a.m. hours, an affected individual feels awkward and lightheaded. There is also a heavyweight and pressure in the head.
Nux Vomica – When sleepiness gets worse after meals
Nux Vomica is considered when sleepiness worsens after meals. Thereafter it is well indicated for seated evening sleepiness that a person is unable to avoid. People who need it sleep soundly and may drop their lower jaws. A violent starting can occur during falling asleep. There may also be talk during sleep.
Causticum – For the treatment of narcolepsy associated with severe daytime sleepiness and nighttime insomnia
People who need Causticum experience severe drowsiness during the day. This is accompanied by yawning and stretching. They are unable to resist and must lie down. At night, there is insomnia with the inability to rest in any position. There is great restlessness at night. They may cry or laugh in their sleep.
Arsenicum Album – homeopathic remedy for narcolepsy treatment in cases of daytime sleepiness while sitting
Arsenicum Album is an excellent remedy for daytime sleepiness while sitting. Constant drowsiness with frequent and violent yawning. twitching of limbs on falling asleep. In the evening, deep sleep occurs where it is required. Tiring dreams appear during sleep. At night there is great restlessness with insomnia. Constantly tossing and turning.
Antimonium Crudum – For drowsiness with head tremors
Antimonium Crudum is a beneficial remedy for drowsiness accompanied by shaking of the head. There is a strong desire to sleep during the day accompanied by heat. Numbness in the head can also be there. It is also indicated when there is drowsiness after eating. Finally, it is of great help when there is great drowsiness in the morning.
Zincum Metallicum – for a continuous willingness to sleep during the day
Zincum Metallicum is useful in cases where there is a continuous disposition to sleep during the day. Overwhelming sleep occurs. Sleep is deep with many dreams. Frequent jerks and jerks are felt during sleep. At night it is difficult to fall asleep. Sleep doesn’t bring the feeling of rest and is frequently broken during the night. Screaming in sleep can be there. In the morning, the person does not feel rested.
Pulsatilla – for irresistible drowsiness in the afternoon
Pulsatilla is a natural medicine made from the plant Pulsatilla Nigricans. Belongs to the buttercup family. Its use is recommended for insurmountable drowsiness during the day. Sleeplessness at night, with extreme restlessness. Insomnia is most pronounced in the first half of the night. A sound sleep comes when it’s time to get up. On waking, one feels weak and unrefreshed.
Sepia – Use it as a Natural treatment for narcolepsy when there is daytime sleepiness right after sitting down
Sepia is an important medicine when there is excessive sleepiness during the day and the person falls asleep as soon as they sit down. He doesn’t want to get up and has a hard time waking up. With this, one could speak aloud in sleep. At night he wakes up scared screaming. After sleep, at night there is fatigue, pain, and a feeling of non-freshness.
Natural treatment for narcolepsy in Philadelphia
Rare diseases such as narcolepsy are geographically dispersed, resulting in limited knowledge about diagnosis and treatment. WHO has initiated global efforts to promote research, development, incentives, and commercialization of orphan medicines in the EU and US.
Although narcolepsy is a rare disease, if left untreated or undiagnosed, it can have a negative impact on the quality of the workforce while also impairing an affected person’s social, cognitive, and psychosocial functioning.
The aim of this blog post is to increase awareness and knowledge on this topic. More countries should initiate research on this topic and work towards setting up treatment centers for affected populations.
Holistic treatment for narcolepsy is effectively provided by the team of medical practitioners at the Philadelphia Holistic Clinic under the supervision of medical doctor Victor Tsan.
To schedule, an appointment for holistic evaluation contact our clinic at
(267) 403-3085
or use our secure online application.
Comments
Post a Comment