Contents hide
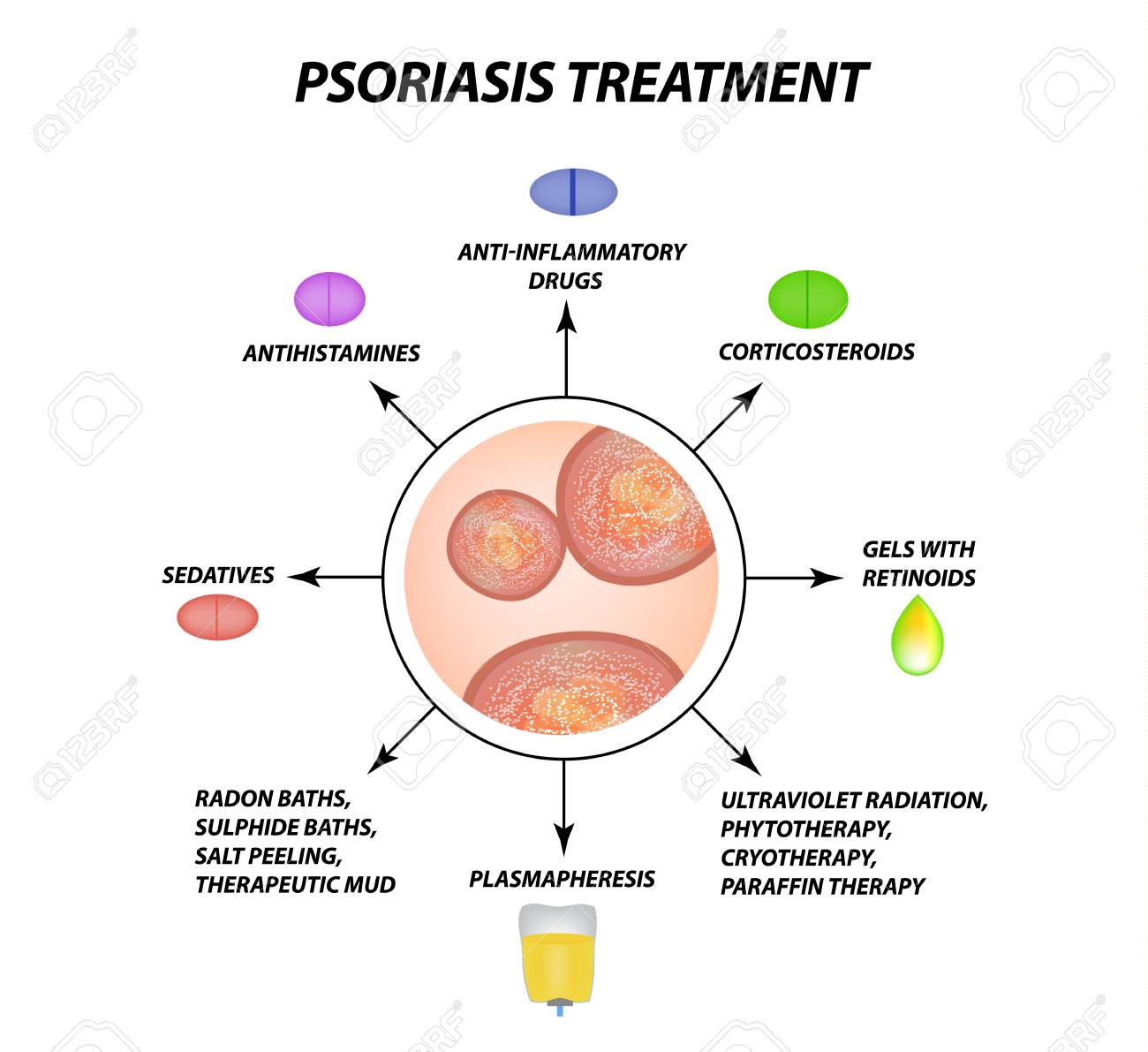
Treatment of psoriasis
Treatment of psoriasis aims to stop the skin cells from growing so quickly and to remove the scales. Treatment options in western medicine include the use of creams and ointments (topical therapy), phototherapy, and oral or injectable medications.
Which method of treatment for psoriasis you will use depends on how severe the symptoms of psoriasis are, and how the disease responds to previous psoriasis treatments. You may need to try different medications or a combination of different therapies before finding an approach that works for you. Usually, however, the disease returns after some remission that may last from a few weeks to a year.
Topical treatment of psoriasis – the most common traditional approach.
Corticosteroids.
These ingredients are the most commonly recommended by dermatologists medicines for the treatment of psoriasis while the disease is in mild to moderate form. Corticosteroids are offered in a form of balms, emulsions, lotions, gels, creams, foams, sprays, and shampoos. Mild hormonal ointments such as hydrocortisone are usually recommended for applications to sensitive areas on a face or skin folds, and to treat large plaques. Topical hydrocortisone can be applied once a day during flare-ups, and every other day or on weekends only to maintain remission.
Your dermatologist may suggest a stronger steroidal liniment or ointment such as triamcinolone, acetonide, Trianex, or Temovate for smaller, less sensitive, or more stubborn areas.
Long-term or excessive use of potent corticosteroids can thin the skin. Over time, topical corticosteroids may stop working.
Vitamin D.
Synthetic forms of vitamin D, such as calcipotriene calcitriol, and Vectical, reduce the speed of growth of skin cells. This type of medication can be used alone or along with topical corticosteroids. Calcitriol may lead to relief of irritation in delicate areas.
Retinoids.
Tazarotene, Tazorac, and Avage come in the form of a gel and cream and are applied once or twice a day. The well-known side effects of these drugs are skin irritation and augmented sensitivity to light.
Tazarotene is not recommended if you are pregnant, breastfeeding, or about to become pregnant.
Calcineurin inhibitors.
Calcineurin inhibitors, such as Tacrolimus, Protopic, Pimecrolimus, and Elidel, lessen the level of inflammation and plaque buildup. The Calcineurin inhibitors can be exclusively beneficial in areas of thin skin, for instance around the eyes, where steroids and retinoid emulsions and ointments are too irritating or can cause damaging effects.
Calcineurin inhibitors are not recommended during pregnancy or breastfeeding, or if planning to become pregnant. This drug is also not intended for long-term use due to a potential increased risk of skin cancer and lymphoma.
Salicylic acid.
Shampoos and salicylic acid solutions reduce the scalp of scalp psoriasis. It can be used alone or to increase the ability of other drugs to penetrate the skin more easily.
Coal tar.
Coal tar as a medicine used for psoriasis treatment reduces flaking, itching, and inflammation. It is available over the counter or by prescription in various forms, such as shampoo, cream, and oil. These products can irritate the skin. They are also stained clothes and bedding and have a strong odor. Coal tar for the treatment of psoriasis is not recommended for pregnant or breastfeeding women.
Goeckerman therapy.
Some doctors combine coal tar treatment of psoriasis with light therapy known as Goeckerman therapy. The two therapies taken together are more effective than either alone, as coal tar makes the skin more receptive to UVB light.
Anthralin.
Anthralin – a tar product comes in a form of a cream and is used to slow the growth of skin cells. It can also help to remove dandruff and make the skin smoother. It should not be used for psoriasis treatment on the face or genitals. Anthralin can irritate the skin and discolor almost everything it touches. It is usually applied for a short time and then washed off.
Light therapy – effective treatment of psoriasis
Light therapy is a first-line treatment for moderate to severe psoriasis, alone or in combination with medications. This method of treatment for psoriasis involves exposure of the psoriatic skin patches to controlled amounts of natural or artificial light. Repeated light therapy treatments of psoriasis are necessary. Talk to your doctor to find out if home phototherapy is an option for you.
Sunlight.
Brief daily sun exposure (heliotherapy) may improve psoriasis. Before starting a sun regimen, ask your doctor about the safest way to use natural light for the treatment of psoriasis.
Broadband UVB.
Controlled doses of broadband UVB light from an artificial light source can treat single plaques, generalized psoriasis, and psoriasis that does not improve with topical treatments. Short-term side effects can include redness, itching, and dry skin. Regular hydration can help ease your discomfort.
Narrowband UVB.
Narrowband UVB light therapy may be more effective than broadband UVB therapy and has replaced broadband therapy in many settings. It is typically directed two or three times per week until the condition of the skin improves, and then rarely for supportive maintenance. However, narrow-band UV-B phototherapy can cause more severe and prolonged burns.
Psoralen plus ultraviolet A (PUVA).
This treatment of psoriasis involves taking photosensitive drugs (psoralen) before exposure to UVA light. UVA light penetrates the skin deeper than UVB light, and psoralen makes the skin more susceptible to UVA.
This more aggressive psoriasis treatment permanently improves the condition of the skin and is often used in more severe cases of the disease. There are some known short-term side effects listed below:
- nausea,
- headache,
- burning, and
- itching
Long-term side effects include dry and wrinkled skin, freckles, increased sensitivity to the sun, and an increased risk of skin cancer, including melanoma.
Excimer laser.
For this form of light therapy, strong UVB light is only aimed at the affected skin. Excimer laser therapy requires fewer sessions than traditional phototherapy because it uses stronger UVB light. The most common side effects are redness and blistering.
Oral or injected medications for the treatment of psoriasis
If you are suffering from moderate to severe forms of psoriasis or if other treatments for psoriasis have not worked, your doctor may prescribe either oral or injectable (systemic) medications. Due to the potential for serious side effects, some of these medications are only used for a short time and may be used alternately with other treatments for psoriasis.
Steroids.
If a few small, persistent psoriasis patches appeared on your skin, your dermatologist may suggest injecting triamcinolone directly into the lesions.
Retinoids.
Acitretin aka Soriatane and other retinoids are pills prescribed for the treatment of psoriasis, aim to reduce the production of skin cells. Side effects can include dry skin and muscle pain. These medicines are not recommended when you are pregnant or breastfeeding or if you intend to become pregnant.
Methotrexate.
Usually given weekly as a single oral dose, methotrexate and Trexall decreases skin cell production and suppresses inflammation. It is less effective than adalimumab (Humira) and infliximab (Remicade). This can cause an upset stomach, loss of appetite, and fatigue. People who take methotrexate long-term need continuous tests to monitor their blood counts and liver function. The use of Methotrexate represents the more aggressive strategy of treatment for psoriasis.
Both men and women should stop taking methotrexate at least three months before trying to conceive. This medication is not recommended when you are breastfeeding.
Cyclosporine (Neoral).
In cases of severe psoriasis, taken orally, Cyclosporine suppresses the immune system. It is similar to methotrexate in terms of effectiveness, but cannot be used continuously for more than a year. Similar to other immunosuppressive medicines, cyclosporine increases the risk of infection and other health problems, including cancer. People taking cyclosporine for the treatment of psoriasis need continuous monitoring of blood pressure and kidney function. These medications are not recommended during pregnancy, breastfeeding, or if you plan to get pregnant.
Biologicals.
These drugs, used for the psoriasis treatment usually given by injection, alter the immune system in ways that disrupt the cycle of illness and improve symptoms and signs of illness over several weeks. Some of these drugs are approved for the treatment of moderate to severe psoriasis in people who have not responded to first-line therapy. Treatment options are expanding rapidly. Examples include Etanercept (Enbrel), Infliximab (Remicade), Adalimumab (Humira), Ustekinumab (Stelara), Secukinumab (Cosentix), and Ixekizumab (Talz). These types of drugs are expensive and may or may not be covered by health plans.
Biologics for the treatment of psoriasis should be used with caution because they carry the risk of suppressing your immune system in ways that increase your risk of serious infections. In particular, people taking these drugs must be tested for tuberculosis.
What is psoriasis

Psoriasis is a chronic illness. It is non-contagious and doesn’t transfer from one individual to another. In the core of the disease, we find autoimmune disorder which disturbs the skin, nails, and joints. It usually results in red or pink, but sometimes even white crusty spots that are seen on the skin, especially on the knees and elbows. These flaking and sometimes peeling blotches are triggered by psoriasis. We call them “psoriatic plaques” and they appeared as a result of a particular psoriatic form of inflammation that causes extreme, unnecessary, and unproportioned skin creation. The derma of the impacted areas swiftly accrues and becomes silvery-white. Plaques often take place on the skin of the elbows and knees. In many cases, however, we can observe the patches in other areas of the body including the skin of the head and genitals. Psoriasis is a persistent skin inflammation, the foundations of which are quite uncertain. This medical disorder is neither results from viruses or bacteria nor it caused by any other internal or dermatological ailments. Psoriasis may impact either men or women and can strike individuals at any time of life.
Psoriasis in its different forms is a relatively common disease, disturbing a little more than two and a half percent of people worldwide. While individuals that have minor symptoms and usually aren’t aware of having this skin condition, the real percentage of psoriasis per capita is above 3.5 – 4. As I mentioned before this skin disorder may start at any period of life, however, ages of 20 – 25 and 50 -60 are most vulnerable.

Psoriasis is a chronic disease that undergoes stages of remissions and worsening and is incurable according to western medical protocols.
Besides the skin itself, fingernails and toenails are commonly impacted by this disease and we call it psoriatic nail dystrophy. In some stages of development, psoriasis may lead to joint pain, rigorousness, and stiffness. This form of psoriasis is identified as psoriatic arthritis. Opposite of eczema that develops in the skin folds, psoriatic elements are more likely to be localized on the outer sides of the joints.
What causes psoriasis
The causes of psoriasis in western medicine are virtually unidentified. Psoriasis is believed to be an immune system problem that causes the skin to heal faster than normal. In the most common type of psoriasis, known as plaque psoriasis, this rapid cell turnover causes scales and red spots to form.
What makes the immune system malfunction is not completely understood. Scientists have faith in the theory that both genetic and environmental influences play a role. While experts don’t know what are the principal causes of psoriasis, we do know that the immune system and genetics play an important role in its development. We know one thing: psoriasis is not contagious. You can’t get psoriasis from someone else. Generally, factors are causing the symptoms of psoriasis to appear or worsen.
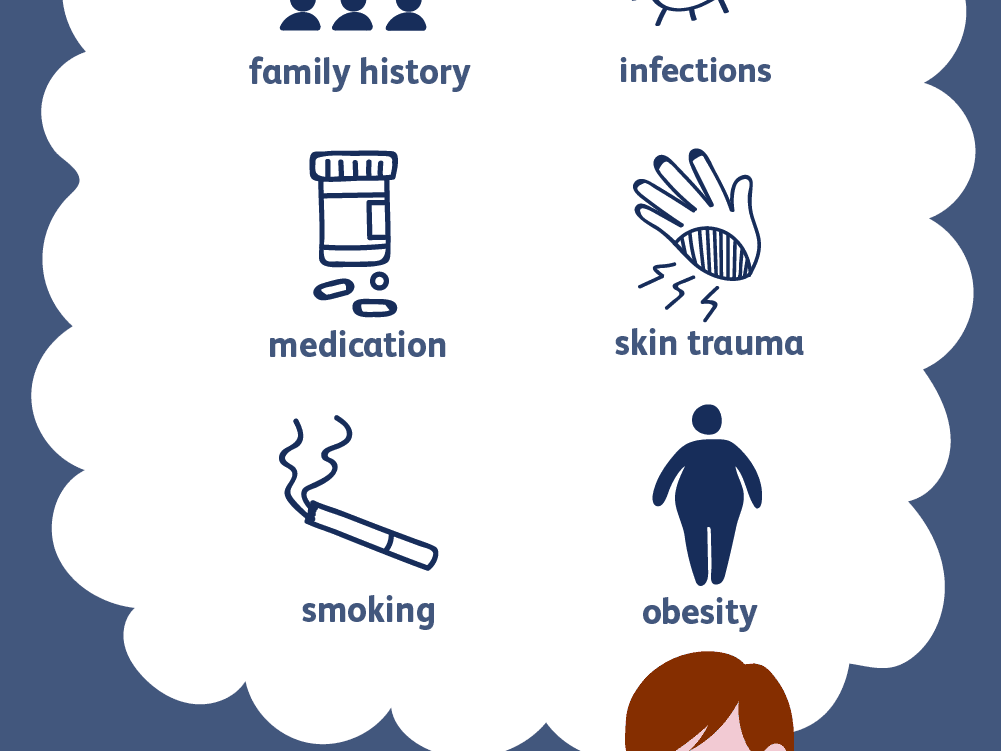
Those triggers may vary from person to person. However, some factors that can trigger, initiate or deteriorate psoriasis are:
- Genetics – Individual, whose parent is suffering from psoriasis have 15% more chances to be affected by the disease. When both parents have psoriasis, 60 percent of their children have a tendency to be also impacted.
- Repeatable and chronic throat infections,
- Skin injuries, bruises, wounds, and cracks,
- Some pharmaceutical drugs and industrial chemicals
- Nicotine and alcohol consumption,
- Emotional trauma,
- Disturbance of metabolism of amino acids.
- Acute and Chronic infections.
Types of Psoriasis
The skin symptoms of psoriasis may have different appearances, locations, and forms. Deviations of psoriasis are:
- plaque,
- pustular,
- guttate
- flexural

Plaque Psoriasis (Psoriasis vulgaris)
The most usual type of psoriasis is plaque psoriasis, which impacts 80 to 90% of all psoriasis patients. Plaque psoriasis typically looks like elevated patches of irritated derma shielded by the old bleached flaking skin. These spots we call psoriatic plaques.
Flexural psoriasis (inverse psoriasis)
Flexural psoriasis manifests as flat reddened spots on the skin. It commonly takes place in the skin bends, mainly between the thighs and groin areas, in the underarms, under the bends and folds of an abdomen wall, and under the mammary glands. This type of psoriasis is worsened by rubbing and perspiration and is at risk of mycological contaminations.
Guttate psoriasis
This type of psoriasis is described by scientists as plentiful round plaques that need to be differentiated from Pityriasis rosea. These multiple lacerations develop over big parts of the human body, such as the head, chest, back, arms, and legs. Development of guttate psoriasis linked to ENT infection especially in the pharynx and larynx, and especially if caused by streptococci.
Pustular psoriasis
This type of psoriasis looks like elevated pustules filled with white non-infectious discharge. The skin around these skin elements is sore and reddish and painful. Pustular psoriasis also is known as palmoplantar pustulosis most commonly manifests on hands and feet.
Nail Psoriasis
Nail psoriasis creates an assortment of symptoms located on nails of either fingers and toes. Those symptoms of psoriasis of this type are:
- discoloring and solidifying of the skin under the nail plate,
- cracks and stripes through the nails,
- the distraction of the nails,
- detachment and decaying of the nail from the nail bed.
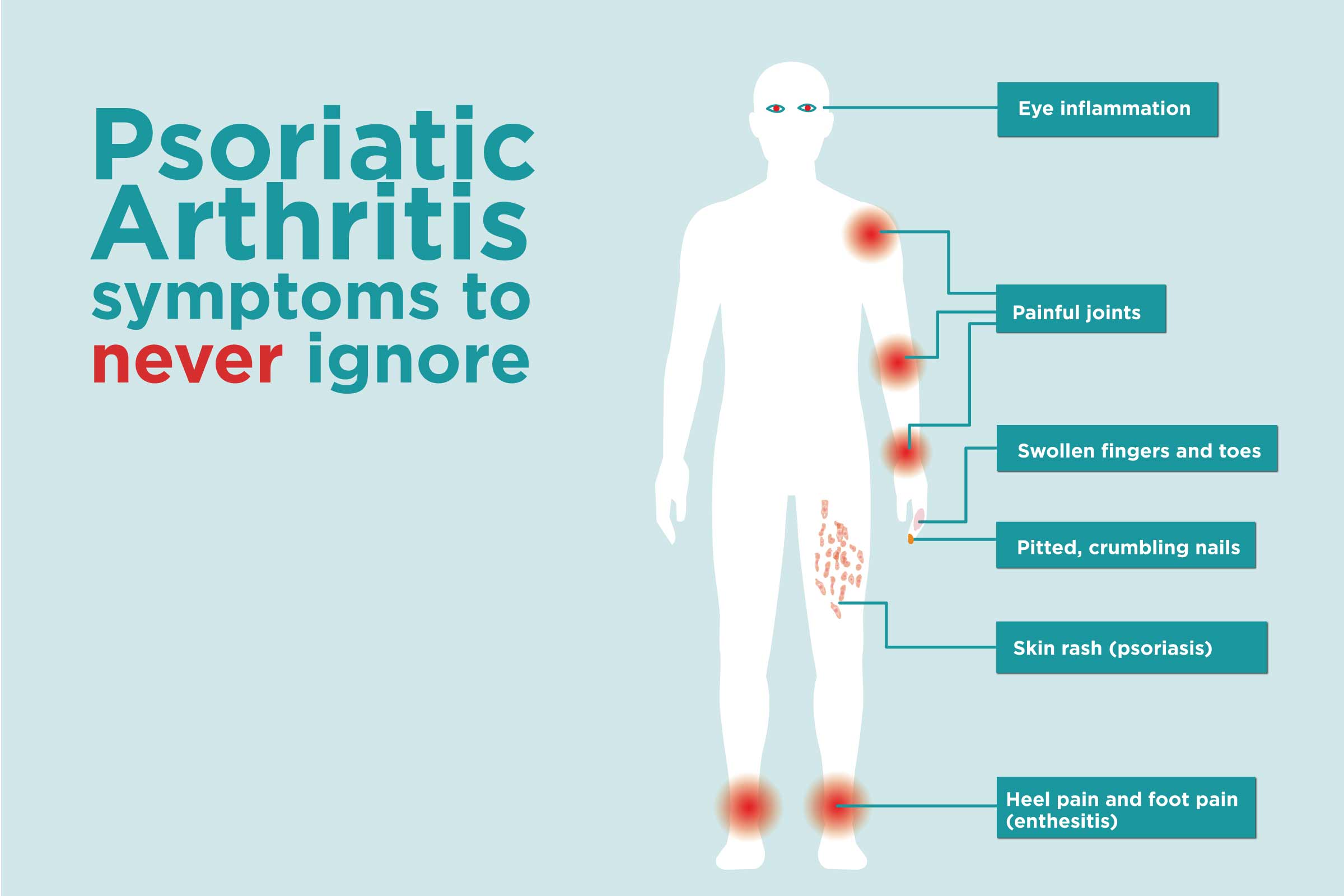
Psoriatic arthritis
This type of arthritis develops as a result of psoriasis and implicates connective tissue (ligaments, joint bursae) and joint inflammation. It may impact any joints but usually small joints of the fingers and toes causing dactylitis (the condition when fingers and toes look like sausages due to swelling. Nearly 10-15 percent of the psoriasis sufferers also report symptoms of psoriatic arthritis.
Erythrodermic psoriasis
Erythrodermic psoriasis embroils the great tenderness, redness, and soreness, as well as exfoliation of the derma. It may go along with severe burning, puffiness, inflammation, and throbbing. Erythrodermic psoriasis is the only type of psoriasis that may be lethal, as the life-threatening tenderness and irritation along with exfoliation interrupt the body’s aptitude to normalize temperature.
Proper diagnosis – the first step to successful treatment of psoriasis
A diagnosis of psoriasis is typically concluded by the look of the skin. No distinctive blood work is required for the diagnostic of this condition. In most difficult cases a biopsy, or scratching of the plaques, may be administered to rule out some additional conditions and to authorize the diagnosis of psoriasis. Skin samples taken from the plaques for the morphological test will discover battered Rete pegs if the sample is affirmative for psoriasis. Also while scrapping the surface of the plaques, bleeding from the derma below the plaque is a positive sign of psoriasis also known as Auspitz’s sign. Homeopathy for psoriasis requires more specific diagnostic in order to find the similarity between the treating agent and the clinical symptomology.
Complications of psoriasis
If you suffering from psoriasis, you are at greater risk of developing other ailments, including:
- Psoriatic arthritis, which causes pain, stiffness, and swelling in and around the joints
- Eye conditions such as conjunctivitis, blepharitis, and uveitis
- Obesity
- Type 2 diabetes
- High blood pressure
- Cardiovascular disease
Natural treatments for psoriasis
People who are looking for alternatives to their psoriasis treatment typically fall into three categories:
1) they want to go the holistic path from the start,
2) have tried conventional treatments such as corticosteroids or immune-suppressing medications without success, or
3) conventional treatments acted on them, but the side effects were too great for their body.
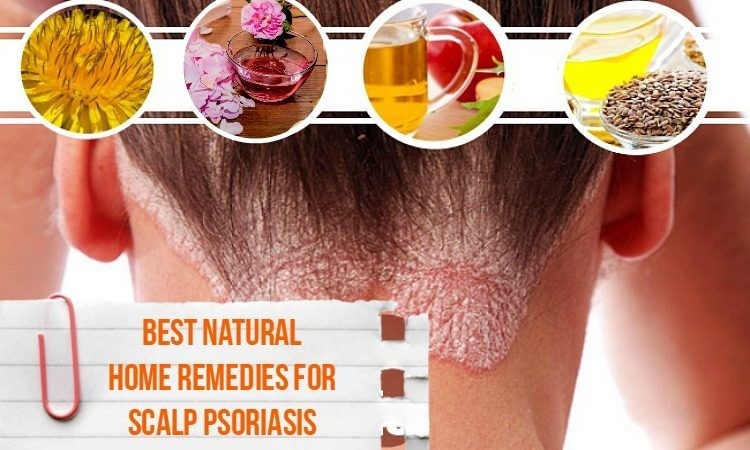
A number of alternative treatments for psoriasis claim to relieve the symptoms of psoriasis. The list of natural remedies for the treatment of psoriasis includes:
- special diets,
- creams,
- supplements,
- acupuncture,
- herbs, and
- homeopathy
The majority of alternative psoriasis treatments are generally considered safe and can relieve itching and flaking in people with mild to moderate psoriasis. Some home remedies for psoriasis are useful in avoiding triggers of the disease’s deterioration, such as stress, depression, intoxication, etc.
Home remedies for the treatment of psoriasis

The home remedies for psoriasis don’t replace treatments prescribed by a doctor, but they can certainly play with your medications – or even work on their own for mild flare-ups:
- Stay hydrated. Yes, it’s common because it works. Remember to use thick fragrance-free creams and oils to keep dander away without irritating your skin.
- Take a bath. Soak your body in colloidal oatmeal or Epsom salt. It’s calming * and * relaxing!
- Watch what you eat. What goes in must come out… and sometimes it comes out as a push. Eat fewer flare-ups by eating fruits, vegetables, and healthy fats instead of red meat, dairy, and gluten.
- Try the supplements. Some people with psoriasis swear by turmeric and fish oil. Just check with your doc before trying them out.
- Zap scalp psoriasis with zinc. Do you know those special medicated shampoos? They are infused with anti-inflammatory zinc!
- Be gentle. Gentle in all aspects of your life and all ways. Choose mild, fragrance-free soaps and lotions. Avoid stressful situations that can trigger a flare-up. And be gentle with your emotions. Psoriasis can be frustrating and isolating, so see a friend or doctor if seizures get you down.
Diet – an essential part of the treatment of psoriasis.
It is important to remember that psoriasis is a chronic inflammatory disease. So, it is important to avoid nutriments that promote inflammation in the body. Warning: the diet should never be dogmatic. What works for one person’s body may not be as good for another’s body.
The age-old debate about eating meat versus not eating meat is a prime example. Some people feel healthier and better when they don’t eat animal protein, while others react exactly the opposite. The idea is to figure out what works for your body.

When trying to figure out what triggers your psoriasis, an anti-inflammatory diet is a great place to start. The straightforward rules for an anti-inflammatory diet are as follows:
- It a rich in vegetables and fruits, healthy fats, lean protein, whole grains, and lots of fresh produce. In other words, a Mediterranean diet.
- Certain foods should be avoided because they tend to promote inflammation. These foods include:
- Dairy
- Nightshade vegetables (tomatoes, potatoes, eggplants, peppers, etc.)
- Eggs
- Gluten
- Refined sugars
- Alcohol
- Processed foods
The main goal of the diet is to avoid entirely probable triggers (pro-inflammatory foods) for about 3-4 weeks. Once you’ve done this and your symptoms have calmed down overall, you start reintroducing the foods you avoided one by one. You will reintroduce a new food every 3 days and it is important to keep track of how your body is feeling during this time. This allows you to succinctly identify which foods are causing flare-ups for your psoriasis.
Acupuncture – an ancient Chinese treatment of psoriasis
One of the main features of Chinese medicine theory is its focus on treating an underlying pattern rather than treating a specific disease. In this sense, TCM does not have an established protocol for the diagnosis and treatment of psoriasis. Instead, it has a set of differential diagnoses and treatment protocols for specific manifestations of symptoms in the general category of skin diseases.

The following are the different diagnostic models that may be applicable to a patient with psoriasis:
- The Blood-heat: “red spots or papules that quickly enlarge and multiply. Red scales accumulate and are easily shed if scratched. “
- Blood deficient and dry: “pale and very dry plaques covered with a thin layer of white scales.”
- Blood congestion: “dark purple skin elements shielded by thick scales.”
- Moist heat: “Dark red macules or papules covered with fatty or thick, crusted scales. The skin cries. There may also be pustules.
- Toxic Heat: “erythematous or pustular abrasions that develop and spread swiftly, frequently gathering on top of each other. There are red scales that fall off easily and there is itching, burning, and pain.
In clinical practice, we find that the patient presents a mixed pattern. This means they don’t fall into a single pattern of blood heat or toxic heat. Very often they show two or more of these designs at the same time. It is then up to the physician to identify which pattern is more dominant in the patient’s presentation and appropriate treatment.
Acupuncture treatment of psoriasis has been shown to promote the release of natural pain relievers in the body, reduce inflammation, relieve stress, and improve blood circulation.
Traditional Chinese Medicine in general and acupuncture particularly can decrease the severity of the following symptoms of psoriasis:
- Red, burning skin lesions
- itching
- Dry, flaky, flaky skin
- Joint pain
- Depression and anxiety
You might be surprised to see depression and anxiety on the list. However, the fact is that many people with psoriasis suffer emotionally: they often report anxiety, depression, shame, low self-esteem, etc.
Acupuncture treatment of psoriasis can have wonderful regulative effects on the nervous system and help individuals reduce stress and anxiety. It is precisely for this reason that many Western doctors are open to acupuncture. The effect of acupuncture on reducing stress is well documented. Because emotional tension, apprehension, and anxiety can make autoimmune diseases worse, many physicians are open to their patients trying acupuncture for its sedative effects.
During the treatment itself, you will likely lie on a bed or table with a sheet or blanket to keep you warm.
Your acupuncturist will gently insert sterile, hair-thin needles into the skin around the problem areas. Expect needles to be inserted 1 to 3 inches deep.
You will then rest with the needles in your body for 20 minutes or longer. This is when the “magic” happens – in other words when the treatment should call qi (energy) into the treated area, stimulating your immune system.
When the time is up, your acupuncturist will gently remove the needles, safely discard them (disposable needles), and then send you on the road.
Friendly Reminder: Acupuncture treatment of psoriasis is not a quick fix. It’s okay to attend multiple sessions before you see an improvement in your symptoms. One of our patients, for example, a young woman went through 13 procedures over 6 weeks before she experienced a difference in her psoriasis symptoms.
Herbal medicines for the treatment of psoriasis
Chinese medicine also relies heavily on the use of herbal recipes to help the body recover naturally. Different herbs have different properties and effects on the body. The key is the use of herbs that treat the patient’s condition.
We talked about clinical pictures earlier in the article. However, there is no single treatment for psoriasis. The two people with psoriasis can present themselves with different symptoms and thus different clinical pictures. A person with redder and burning psoriasis lesions will need different herbs than a person whose psoriasis is very pale, dry, and scaly.

The key is to distinguish and identify the appropriate pattern.
Many of the herbs used in psoriasis have a heat-clarifying effect. In other words, those medicinal herbs stimulate an anti-inflammatory mechanism.
The theory behind anti-inflammatory herbs is that they allow the skin to heal by disrupting the chronic inflammatory process that is continuously damaging the skin. This will help reduce burning, redness, and plaques on the skin.
Homeopathic treatment of Psoriasis
Homeopathy for psoriasis attracts more and more patients since western medicine proved its ineffectuality in this area of dermatology. Homeopathy for psoriasis is as complicated as any other approach, however at Philadelphia Homeopathic Clinic, we documented many successful cases and statistically, the effectiveness of homeopathic treatment for psoriasis is above the nationwide average.
Homeopathy for psoriasis is also highly demanded by patients because homeopathic pharmacopeia is based on natural, organic ingredients in microdoses, which is a significant advantage compared to the administration of long-term steroids’ therapy.
- Arsenic,
- Arsenicum Iodatum,
- Borax,
- Calcarea Sulphuricum,
- Chrysarobinum,
- Graphites,
- Kali Arsenicosum,
- Kali Bromatum,
- Lycopodium,
- Mercurius Solubilus,
- Nitric Acid,
- Petroleum
- Psorinum
- Sulfur
ARSENICUM-ALBUM
The look of the derma is dehydrated, coarse, flaking, dirty, and desiccated. The outbreaks are commonly acuminate with extreme shedding. There is an intense burning feeling in the flare-ups which increases in the late afternoon, at nightfall, and between 1 and 4 o’clock in the morning. The cold application also causes the worsening of the burning sensation. Warm heating pad, opposite, improves this symptom,
ARSENICUM IODATUM
The plaques are written off as noticeable, severe peeling of derma in big scales resulting in an exudating skin layer underneath it. Patients report a severe itching and boiling sensation. These individuals scratch the skin elements aggressively until they start bleeding. The form of psoriasis that requires ARSENICUM IODATUM deteriorates during the dry, frigid time of the year.
BORAX
The derma of hands and head shielded by numerous psoriatic outbreaks. The lacerations usually ulcerate, mainly from minor wounds. The form of psoriasis that may be successfully treated with Borax deteriorates in warm time and improves during the cold season. This version of the disease usually upsets extremely anxious people that suffer from phobias, fears and become scared from unexpected loud sounds.
CALCAREA SULPHURICA
The flare-ups of this form of psoriasis are mainly situated on the scalp, limbs, and torso. The look of the plaques is cherry red with thickening and hardening of the nearby derma. The severity of itching and burning sensation worsens in warm, closed areas (room, apartment, cabin, car, etc.) or from a warm wash in a bathtub or even warm shower. At the same time, patients feel much better from cold applications and cold showers.
GRAPHITES
Pleats of the derma such as external ears, gluteus, groins, the skin of the internal parts of joints are the most common locations for outbreaks of psoriatic plaques of this form. The flare-ups are completely dehydrated and desiccated with slight shedding but more intensive cracking. The crashes hemorrhage effortlessly and give out sticky exudate. The local heat deteriorates the symptoms. This form of psoriasis is usually observed in overweight, constipated patients, whose skin looks dirty. Psoriatic outbursts alternate with gastrointestinal symptoms.
SULFUR
This remedy is the most popular in the dermatological practice of each homeopath. The derma is dehydrated, bumpy, wrinkly, and flaking. The outbreaks may appear on virtually any area of the skin.
The following appearances of flare-ups are typical for Sulphur and indicate the necessity to administer this remedy:
- voluptuous ferocious itching
- symptoms intensified during the night time, in bed,
- worse from rubbing and bathing,
- burning appears and increases from itching,
- worsening throughout the springtime and in a moist climate,
- psoriasis progresses following another dermatological condition that was treated using topical creams,
- psoriasis accompanies other medical conditions such as hay fever, bronchitis, asthma, etc.,
- the typical Sulphur patient is stoop-shouldered, untidy, lanky, and bony, with an unpleasant body smell.
Homeopathic treatment of psoriasis by Dr. Tsan at Philadelphia Homeopathic Clinic
Homeopathic treatment of psoriasis, this serious and non-curable disease, often is more effective than the regular western approach.
Dr. Tsan has extensive academic and clinical experience in homeopathic treatment for psoriasis. Since Philadelphia Homeopathic Clinic is a division of Philadelphia Holistic Clinic we have all holistic services available to each patient. All medical providers at the clinic are licensed and insured. The acupuncturists, herbalists, and reiki practitioners are working under the strict supervision of medical doctor Victor Tsan. To schedule an appointment for holistic evaluation and discuss with Dr. Tsan and ask if homeopathic psoriasis treatment is your best alternative choice contact our office at (267) 284-3085 or use our online scheduling web page
Comments
Post a Comment